Strength on a National Level | Scott Knoer, PharmD and Antonio Ciaccia, APhA & 3 Axis Advisors
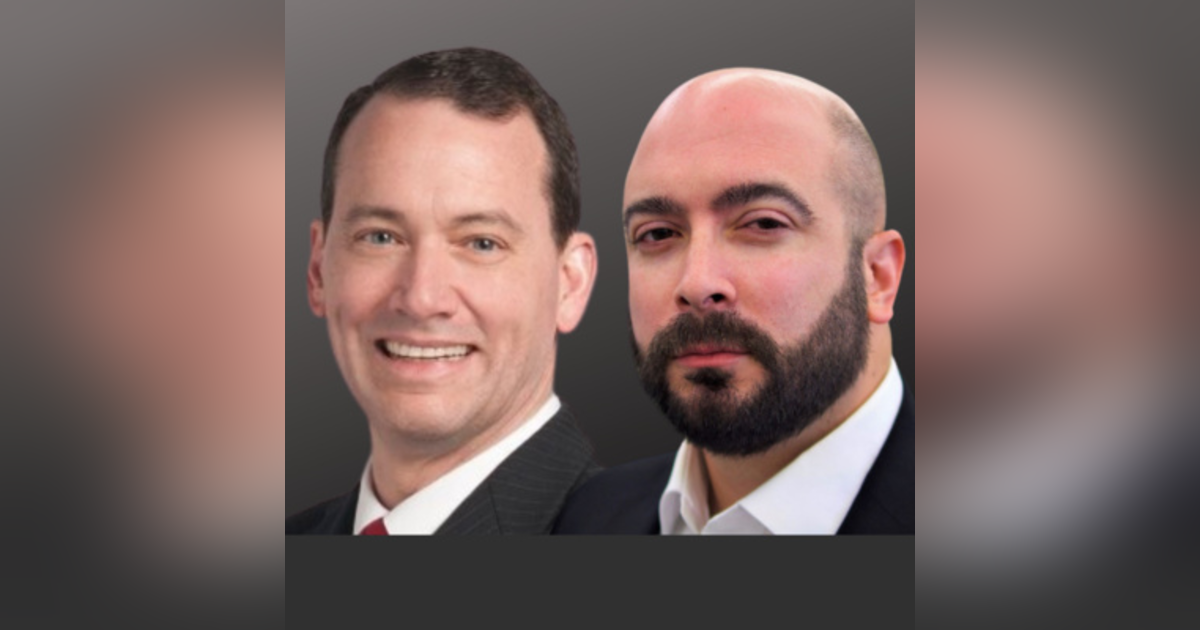

Scott Knoer and Antonio Ciaccia discuss the advantages and challenges of fighting for pharmacy on a national level.
https://www.pharmacist.com/
https://www.3axisadvisors.com/
Speech to text:
Mike Koelzer: [00:00:00] Scott and Antonio, for those that haven't come across you before online, introduce yourself and tell our listeners what we're talking about today
Antonio Ciaccia: at Antonio Ciacca. I am the CEO of 46 Brooklyn research. I am the president of three access advisors. I am also in that capacity and a senior advisor to a number of organizations like the American pharmacist association.
Scott Knoer: I'm Scott Knoer. I'm the CEO of the American pharmacy association here. I don't know, about 18 months, ish, somewhere around there. Last time we talked, Mike, I think we're talking about what are you going to do? And I think we got some stuff I can talk about what we've been doing and where we're going.
Mike Koelzer: I was the president of our local association.
It's one of those things where everybody else who was on the board already runs their turn. And they said, well, uh, what the hell let's give Kelzer a shot, but I enjoy having some comradery as an independent with the other pharmacies in town. And unfortunately I enjoy it sometimes because when I feel like the ship is sinking, I can look at the other suckers that are going down with me and say, well, at least we're going down together.
Now when I look at the APH, is this just a big group of people that can give me some solace instead of going down in a rowboat, we're going down in the Titanic or do you have. Some things you're doing to stop that.
Scott Knoer: Well, definitely my good question. And we absolutely need to fundamentally change the payment model in the United States because we've been, we've been kind of going down in, in community pharmacy, uh, for a long time now with any industry, you know, Trailblazers and leaders who are doing good stuff.
And, uh, we're, we're making our way through that. And we'll talk a little bit more about how we're attempting to really, uh, transform the payment model so that we can be remunerated for the right things and actually have the right incentives right now, as you know, like, uh, in community. Uh, whether it's independent of your chain, it's because of PBMs and DIR fees and other things.
Um, the remuneration has shrunk over the years so much that, uh, you know, and all we're doing is running as fast as we can on the treadmill and, and man in the drive-through window. So getting pharmacists paid for doing the right things, uh, will allow us to, to do what we went to school for, you know, and then you can help manage.
Diabetes and hypertension and keep patients healthy. But right now they're not paid for that. So we are running on the treadmill, but we've got a lot of things in the works.
Mike Koelzer: Are there strength in
Scott Knoer: numbers? Oh my God. Yes. And I would say yes, yes, yes. Um, and then probably yes, but you know, we need to, to, to work together and, uh, that's both, uh, having folks be members of organizations, like APHL.
And, uh, the organizations, the national organizations are really working with each other quite a bit, but, you know, we can't do it. Antonio is out there fighting the good fight. I'm fighting the good fight. Uh, but you know, the more folks are out there and we're a membership organization, right? So without members, we aren't successful.
And, and when we have more members, we can just really sort of blow it up and have a lot more people involved, a lot more people calling legislators and, uh, and working it all over.
Antonio Ciaccia: Yeah, I'll I'll I'll build it up. Mike, what, you know, previously I was with the Ohio pharmacists association. That's where I got my start.
And I can tell you that the profession of pharmacy, uh, suffers from two main things. And one is that the profession is misunderstood and underappreciated. If you ask a lay person what a pharmacist does, you're going to get a very simple answer in return. Uh, they, you know, they check the medications is basically what you'll hear.
Pharmacists, obviously do a lot more than that because of that lack of that perception of, uh, of a minute, a minimal value relative to the actual value. Pharmacists have a struggle in being a loud enough voice in a crowded room of other healthcare professionals whose value propositions are arguably better.
Understood. Combine that with the fact that pharmacists suffer from. I believe I have a very high degree of apathy. It's not just that they don't join a PHA, it's that they don't join a PHA NCPA, their state organization, and so on and so on. So pharmacists in general, compared to other health professions, I mean, I used to see it all the time with the dental association.
They've got joint rates from about 70 to 80% of their, of their respective constituencies, pharmacy. You're lucky to crack a third of all licensed pharmacists who belong to.
Mike Koelzer: Antonio, I'm going to maybe state the obvious that people will say, well, of course it's independence would join because they have more autonomous care of their own self.
And so they're going to do anything they can and the chain pharmacies don't because they're not leading the store. And so they don't feel they have that connection. Is it that easy of [00:05:00] an answer or is there more to why pharmacists are below the rates of dental and things like.
Scott Knoer: I'll start with that a little bit, Mike, and, and, you know, we have seen an increase in our numbers of pharmacists at APHL over the last couple of years.
Uh, I like to think that, uh, you know, people are the message of, of what we're doing and actually accomplishing is, is resonating with people. But our board is really diverse. You know, I've got some community farmers. Owner's, I've got people from academia, I've got, you know, all kinds of pharmacists, uh, uh, you know, from, from various backgrounds.
And, uh, I think that's important. You know, we are the only organization that represents pharmacists in all practice settings. You know, the chain pharmacists to Mike. I think they've just felt that in a lot of places it's too stressful. All the crazy stuff that's happening with, with vaccines and what our people are faced with and the increased volume.
Uh, and I, you know, we're, we're doing a lot, I think, uh, we're we're seeing some folks respond to say, Hey, you know, let's, let's have a voice. Uh, we, we don't have to just take what's given to us and we can be a little more proactive. If
Mike Koelzer: this was high school, you guys would still be the new freshmen, maybe sophomores.
Where were you the most naive? Scott coming into this and well, let's say you're a sophomore and Antonio's a freshman. Where were you most naive a year ago? What hits you slash may cause the most stress that you didn't think was going to cause.
Scott Knoer: A lot of folks really have no idea what, what organizations actually do.
It took a little while to understand people's perspective of where they come from now. I think a lot of that mic is marketing. One-on-one right. APHS is great. Organization has been for, well over a hundred years, they weren't really good at letting people know what they were doing. Right. So I've taken a slightly different approach on that.
Uh, social media and all and doing podcasts. And I think folks are starting to see, you know, wow, wait a minute. These guys are doing a lot. They are advocating, uh, they're, they're creating important, uh, materials for us. So, you know, it's a lot of why people don't know it's, it's our own fault. Right. You know, it's, it's, it's marketing, you know, and if people don't know it didn't have.
Mike Koelzer: And we all have to be easy on ourselves because social media, relatively new in the scheme of things back in the day, if you wanted to promote yourself, you kind of had to preach to the choir
Antonio Ciaccia: almost. Yeah. Mike, if I was a, if I was a freshman, uh, I I'd like to say I was the freshman who came in with a little bit of facial hair, starting to come in.
I was here, I had the trash desk coming into freshman year. You know, where I started was at the state level. And at the state level, I. Like the state is where you can get things done. You know, you can make a good case. You can, uh, you can push and you can actually get things across the goal line. And, Scott, I would agree with this.
And we're like, now that we were thinking that anything's easy because nothing's easy. Well, there were like, we'll take the Ohio playbook over to DC. Fix all this stuff, we'll jam it down their throats and, you know, Hey, everything will be just fine. The one thing that I learned that, uh, I think I wouldn't say I was naive about, cause I was already pessimistic about the federal government is that, you know, Big time, but, uh, the federal government is, is slot.
Like, as you could imagine, and then some, uh, it's just dysfunctional, as you can imagine. And then some, and it is incredibly difficult to get things done at the federal level, which is why, regardless of whether we're talking pharmacy or anything else. You have to, uh, back your strength, the numbers comment. It's really important to have as many people activated as possible.
It's really important to find a coalition of people to support endeavors. And it's really important to use media to your advantage, to amplify issues that don't get enough attention and lastly When all else fails, work really hard at the state level because you can drive momentum in, in places that are more functional to hopefully get momentum and push things at a, at a larger scale in DC.
And we've seen success on that front. Uh, you know, like I think the last time we talked, we talked about how, how unaware people were of what a PBM is, what a pharmacy benefit manager is, what a pharmacist can do as a clinical service. And that's not the case anymore. The federal, the folks at the federal.
Very much understand what PBMs are. They understand where the problems are. They also understand that pharmacists provide a much better value proposition than any one of, as anyone would have assumed before the pandemic.
Mike Koelzer: I know when I was watching Hamilton with my family, I dropped the [00:10:00] boatload of money on that stupid musical.
It's like every time it comes to town or anybody in my family wants to go see the damn thing, it's like, it's on Disney. Now. Just watch it on Disney. Anyway, watching Hamilton, they said that one of the beauties of the government is that the US government is set up on purpose and checks and balances slowly. And that might be fine when you're talking about stuff like amendments and constitution stuff.
All this stuff. I think we get impatient, you know, when you're really talking about day-to-day businesses and that kind of stuff.
Scott Knoer: Yeah. I think you're right, Mike. And you know, I'm actually, uh, to punish myself, I'm listening to the audio book. Hamilton, every time we get on an airplane, it's super loud. Oh, my God.
That's interesting. The details they go into about that guy's life, but, you know, and being in DC, you know, so when I got there, uh, I'd been there, but never spent a lot of time there until I moved out there. You know, you go out to the founding fathers, uh, places you had, uh, you know, uh, Jefferson, Washington, and, uh, and you see.
How bright they were, they'd seen where everyone else had failed and that, that, you know, big picture you're right. It, it, you know, have, and you can see it playing out right now, right? The Supreme court they're talking to, you know, versus Congress and the president, if any one of them gets too much power, then you can go one way, way too far.
And they do have checks and balances, but yeah, that does make things a little slower. And I would say even worse than that, it's just how polarized our country is right now. So, uh, you know, if we are to the. Uh, legislature, you know, we could actually pass some laws, but everything is so, you know, uh, right left and, and, uh, it's, it's really, it's really sort of rough.
So I'm glad we have that separation. And I think that politicization, uh, is so bad right now is what makes it challenging. You know, having said. You know, the government works slowly. We were educating folks, you know, the, the, the, the lessons that we're seeing, you know, Antonio and I worked together in Ohio, uh, and, you know, got Medicaid to pay pharmacists when you got those examples to take. That's great.
And we had some wins with the prep act, you know, and that's the thing. So everyone's like, oh, the prep ed pharmacist can vaccinate pediatric patients in every state and in all things together that didn't happen by magic. Right. APHL and other pharmacy organizations. We're talking. My team talks to health and human services, at least weekly.
I've had a couple of calls with, uh, secretary of viscera myself. They call us, uh, you know, this, this thing with monoclonal antibodies. We were very, very involved with helping them get that the white house. Because my team, uh, going regularly, I, I at least weekly, you know, cause he got a new white house.
They reach out, you know, so it's it's it is. And so I was on with, uh, the chair con of the FTC. Recently twice last month I was personally given wow, uh, statements about the problems with vertical integration. You know, it used to be just insurance companies and PBMs and pharmacies, and now they're buying providers as well.
You know? So, so they're, they're interested. So, you know, and people don't know that, why would anyone know that? Right. But, uh, you know, so the FTC reaches out to health and human services, constantly calls them. Lisa Bernstein, who runs my government. Fantastic. She worked for 31 years with the FDA.
You know, I had 450 people reporting to her. She knows everybody, you know, all the staffers, the political people change over every administration. The staffers are the people who are actually paid to get things done. I guess that's a thing I didn't really realize just how involved we were in trying to get things moving.
And, and that kind of goes back to the thing I said before. A lot of. Pharmacy doesn't have one voice. I think we're a little bit more, one voice than we used to be. I think, you know, EPHA is seen now by a lot of our, a lot of folks to health and human services, uh, as, Hey, these guys represent all of pharmacy and, uh, we're getting their attention, but we work with all those other organizations I tell you with.
Yeah. Every week, uh, Chad wars, CEO of ASC P hosts them all meeting with all the, all the different pharmacy CEOs. And we write letters together and we educate and, uh, you know, we put out op-eds and, and you know, so pharmacy is doing a pretty good job, I think, uh, better than historic of working together
Mike Koelzer: as individual pharmacists.
I know I go through a lot of emotions. I go from. Anxiety someday to anger, to depression. And that's just when I'm talking to my kids in the morning before, just kidding, but you get all these emotions, you know, if I came to you with a real emotion meter and I said, scatter Antonio, what do you feel like today?
Because of this job? Well, what emotion might you
Scott Knoer: feel? I'm a doer and I like to get things done. So, uh, frustration tends to [00:15:00] be the one that hits me the most, you know, uh, you know, you think you got a bill almost introduced and you know, you find out that the AMS screen in the background. And the other thing I gotta do is get over it.
Right. Uh, have my little pity party and then move on. But I'd say that's the, probably the thing, uh, I, I. Honestly, it's, it's exhilarating. It's ridiculously hard work, but I love being here and doing what I'm doing, but, uh, certainly I get, I get frustrated, but, uh, but then I put on my big boy pants and keep moving.
How about you, Antonio?
Antonio Ciaccia: I'm not very emotional. Uh, but I will say there are, there are really two things that, um, that get me there that the Italian starts to like boil inside. Uh, and one is people that, um, Our unnecessarily and undeservingly so territorial, um, a lot of dysfunction is protected by people that are protecting territory that they, they have, uh, No business protecting.
And I will give you an example. We encountered this all the time, whether it's a government agency or an employer where somebody somewhere is overseeing pharmacy benefits for that organization. And we all know. That this system is very complicated. And I always, I often say it's, this is like playing chess against Bobby Fischer.
You are supposed to lose this game. Okay. But you have people that are overseeing it, that either are trying hard or they are trying hard and fail. Or they're apathetic, whatever it is. Okay. But for whatever reason, they are getting overcharged significantly within their pharmacy benefits. They're getting taken advantage of.
But what they do is rather than open the door and say, help me out, or somebody comes in or my broker screws our PBM screw, whatever it is. They're not willing to basically concede that perhaps something is awry. And so what they do is they cut. They bat, they Batten down the hatches. They get in defense mode rather than opening up and saying, Hey, you know what, it's understandable.
This is we're, we're being made to be exploited. Those things really bother me because they don't earn that. Territorialism they don't, they don't get to be that way because they haven't deserved it. Is
Mike Koelzer: That pride? Is it lack of trust? Is it pride? It's pride. I don't need someone coming and telling me this.
Antonio Ciaccia: Yeah, we would all hate it. Right. You know, somebody looking over your shoulder saying that something is, is wrong. The other thing that bothers me a lot is when somebody knows that something is wrong. And they choose not to do anything about it, or they pretend like it doesn't exist. And it's almost in the same bucket, but we encountered this in Ohio.
When the spread pricing problem occurred. And for those that didn't listen to the last podcast in Ohio, we had a problem in our Medicaid managed care program where PBMs acting on behalf of the state's five Medicaid managed care plans were caught, busted. They were busted because they were paying pharmacies very low.
They were billing the state very high in pocketing. The difference. Myself and my colleague at the time, Eric Pacman, who you've had on the show before we helped use data analytics to help uncover what turned out to be a $244 million gap that was living in between the transaction to PBS we're skimming off the top.
We brought that stuff to state officials with the Columbus district. And other state officials and they sat on it, they knew it was a problem. They didn't do anything about it. The problem for me was not that they were, you know, there was $244 million away. So the pharmacy owners would say that was the problem.
My problem was that they knew it was. They knew it was going on and rather than address it or admit to it, they covered it up. And so that's the stuff that bothers me. It's deception.
Mike Koelzer: When you were talking about the speed of the government, is that multiplied in the federal government.
Antonio Ciaccia: It is with an asterisk because the federal government is dealing with a lot of competing interests.
And so let's, let's use an example, Mike, if I was to give you a top five list of the things that bother you, when you're on the calendar as an independent pharmacy owner, my bed is 1, 2, 3, 4, and five would be DIR fees. Sure. And would it be correct?
Mike Koelzer: That's right. Worse than fighting a monster is fighting a monster.
You don't even know what direction they're coming from.
Antonio Ciaccia: And I can tell you the previous administration and the current administration knows and understands pharmacy's problem with DIR fees, but more broadly, they understand the overall problems with DIR fees and how they impact catastrophic coverage in government and the federal government spending.
Well, how it impacts a patient's out of pocket expenses. They understand that there's something very wrong there, but here is part of the problem: DIR [00:20:00] fees. In either entirety or more likely in a large proportionality are being used to offset member premiums, essentially artificially suppressing them.
So when more DIR is created, it is being used to pass along and artificially suppress premiums. What I just said is it is the six subsidizing everybody. It's the exact opposite of the system it is supposed to run. CMS HHS. They know this, but they are balancing that with polet politics, because what happens if they get rid of DIR or they get rid of manufacturer rebates and they move them all to the point of sale.
Well, now those things that have been used to artificially suppress premium. Could be used to, you get rid of them, premiums go up and nobody wants to deal with the political bash backlash of that possibility. So what does that create? Doesn't cowardice be, you could argue it's cowardice and they don't want to tackle it, but you could also say, it's just say, Hey, why rock the boat?
Let's keep the status quo going. That's frustrating. That's noxious. But I wouldn't necessarily say that's as bad as, Hey. I know that our state of Ohio is getting screwed and we're going to do nothing.
Scott Knoer: You know, on that mic, you know, I think another big example with that, it's not the government, but, um, from my experiences, uh, at that, uh, Cleveland clinic and that really, I think all health systems, I think it translates into employers.
Do you know, in a major employer, I mean, pick one, I don't care Microsoft or, or whoever do you do you mean. Uh, or pick a healthcare organization, you know, pick, pick a big health system. Do you know who at that health system is negotiating the contracts for who they choose as a PBM? Who do you think it is?
What department do you think is a pharmacy that knows? You think it's physicians,
Mike Koelzer: I'm going to guess it's somebody like that. Can't see through the smoke and mirrors that the PBMs have put up. It's
Scott Knoer: almost always HR, HR. What does HR know about a pharmacy benefit? Right. So, so they're, they're not clinicians now.
They're not trying to do things wrong, but they have no idea. So, you know, we were attempting, I was attempting before I left to kind of create my own PBM. You know, it's just the lack of understanding. And then they get these rebate checks and it's like a rebate crack to them and they don't understand the big picture.
They don't understand that if we were to capture this own business within our health system, we would control our spending so much, uh, you know, is, uh, it's to me. It's it's my, so that's, that's kinda what Antonio, I think an example. It's frustration ends, not the right people. I mean, pharmacy, that's what we do.
I mean, we understand formulary and we understand drugs. We understand because every health system has got a P and T committee. Right. Decide what your what's on there for the most cost-effective medications, PBMs are not incented to do that. Right. They're incented to make more money. So, you know, that's, that's one of those crazy things that I learned, the hard way that, uh, the wrong.
And I guess it's because it's an employee benefit and benefits or HR, right. To me. Uh that's that's just, that's crazy, but it's almost universal.
Mike Koelzer: They might be the right people for their job, but they're making the wrong decisions, but here's the question. And we want the dirt on this. You guys, as you get into Washington, are there some people in roles, you shake your head and say, how the hell is that person in this job?
Do you see a lot of incompetence? Because I'm always thinking as levels go higher, you get people that sift out and you get better people up there, but do you ever see people that are just, they have no business being there?
Give me an example. We don't need names, but give me an example.
Antonio Ciaccia: I'll I'll I'll, I'll say, I'll say things that Scott said a lot to say. Hey, you know,
Mike Koelzer: Frank's not here babysitting us this time. Scott
Scott Knoer: step on my foot. I'm
Mike Koelzer: not sure if that was for me or for you, but I think it was for you. I think it
Scott Knoer: was for me,
Mike Koelzer: But you don't have to have a babysitter anymore. Congratulations,
Antonio Ciaccia: Mike, why do you think I'm here?
Scott Knoer: That's under other duties as assigned, keep keeps down from.
Antonio Ciaccia: Now, you know, like there are, um, there are people I'll put them in two buckets. There are those that have been there for a really long time and understandably they've been dragged. They are like, they've just been beaten. They've been through these fights a million times, even though the issue changes and the arguments change.
It's the same ones. I'll equate it to when I was in college and I was bartending weddings. Okay. Once you go to a, what you work two or three of them, they're all the same. They're all the same. And so enough folks I think have been there for a long time, get really disenchanted with the process. And so what they do is they just become bumps on a log.
They [00:25:00] stop listening, they stop engaging. They're just there. Those are very frustrating.
Mike Koelzer: We might see that as incompetence, but they might be either passive aggressive or have just given up or something. They may not be incompetent, but they're just, they're not there. Right.
Antonio Ciaccia: And the other, the other, the other kinds are folks who know better and.
And just don't put in the work. Yeah.
Scott Knoer: Yeah, sure. There's, there's incompetent people everywhere.
Mike Koelzer: Scott, don't twist this into the positive. It's not fun to sit here and listen to all the good things you say. We
Antonio Ciaccia: want the
Scott Knoer: dirt. I know. I know. But Mike, you know, I'm honest here. A lot of the people we're working with want to do the right thing and, and me.
Competing priorities. They got politics, but yeah, there's always incompetent dirt, but I swear to God, you know, we're working with folks and again, health and human services and the white house, the FTC that I think want to do the right thing and, and, you know, again, They got competing priorities, you know, they're listening to us, but then they have to listen to the PBMs too, you know?
Cause they gotta listen to everybody and, and you know, so I think I, you know, I, I'm a little bit more optimistic. Um, uh, yeah, it's making sausage, but you know, it's, my life is about relationships, you know what I mean? So, you have to find people who are like-minded, who get. And you have to work around the incompetent folks, but yet you've got to connect with people and get them to see the light and want to change with you.
But you can do that. You know, it's not easy. I'm
Mike Koelzer: kind of toying with you guys because I'm at the store every day and more so now in the last. Six months more than ever. I've heard complaints about our brothers and sisters over at the chain pharmacies, you know, for various reasons, overworked and understaffed, underpaid and all that kind of stuff.
My first thing I say, and I just think it's good marketing on my point. The first thing I say is. Those people are good. Pharmacists, you know, they're good people. They mean well, but you put enough stress on someone and you put them in a situation where they can't perform and they're going to look terrible.
You know, there's some people that are just incompetent, but a lot of it's like we mentioned, you know, it might be. Burned out, whatever. It's not easy out there.
Scott Knoer: We all went to pharmacy school, people who are, you know, uh, in, in jobs where they're stressed and some of those high volume stores, uh, Mike, and, you know, you know, they are, they're good folks, but you know, that goes back to some of the things we're doing.
And I like to think that I'm not so far that you could say, yeah, Scott's in DC, all that, but I'm really trying to stay in touch through my boards, through my colleagues, through my friends. And you know, there's a lot of folks that, um, are, are. Try and do the right things, but, you know, it's the incentives again, right?
It's the payment model. Okay. Uh, you know, name a big chain, but they would have pharmacists doing the right things if they got paid for it. Right. You know, so, and even the big companies that now the ones that are owned by PBM as well, that there's clearly a misalignment of incentives, you know, but, um, you know, for other folks are they're working in, uh, you know, chains, the chains they got.
Their business. Okay. Now, you know, you'd like to think they also are ethical. If they got paid for the right things, they would do it. You know, so back when we were, you know, uh, getting the, the prep X stuff, you know, we were thrilled working with health and human services when they said pharmacists can vaccinate pediatric patients in every state, regardless of state law, you are giving each other high fives around the office, you know, at least and stuff.
And, you know, I'm hearing from folks like Scott, how am I going to do that? You know, and fill an X, a hundred prescriptions. And now I have crying kids. I got to give vaccinations too. And, you know, yeah. So I mean, my, my girlfriend. Her or nine-year-old daughter to get a vaccine, uh, Ohio state, pharmacy student, you know, in local community pharmacy.
Oh my God. She was good. But that took work. I mean, you know, a mean good kid, but was scared and was crying, you know? And, and so the stresses, but now, by the way, Ohio state's teaching something. Right. Cause that, that student was amazing, but you know, but that's the kind of stuff that's where sometimes policy and frontline disconnect.
So that's why it's so important for me to talk to people and understand what's going on.
Mike Koelzer: What do you hear from pharmacists that you think is irrational or illogical or for whatever, the reason we won't judge, but oh, what the heck, whether it's selfishness or holding onto the past too much. What things do you hear from pharmacies as a group where you're like, come on guys.
Not happening. Let's move on. Yeah. I'll I'll,
Antonio Ciaccia: I'll give you a perfect example. You know, when we were, uh, diagnosing a lot of the problems in Ohio was spread pricing. Again, PBMs pay low billing. The difference after spread pricing was banned. Several pharmacies started to get increased reimbursements on a select number of [00:30:00] medications.
So for example, the prescription for generic Gleevec went up about 1762% in March. From the quarter that spread was banned to what it wasn't. So what was happening was PBMs after they were told you can't take the $244 million in the gap said, all right, we'll push that money downstream. And when they pushed it down stream, it just so happened that many of the medications that they got them.
We're medications that were primarily filled through pharmacies owned by the PBMs themselves. So essentially found a way to boomerang the money back to them by overpaying on select medications that were being funneled through their specialty pharmacies. We talk about that a lot today as an issue called patient steering.
So they overpay, they steer the patient and then they capture the margin. Well, I had an independent owner in New York. I was giving a presentation to the pharmacist on the state of the new. An independent order came up to me afterwards and said, you shouldn't talk about those things. You shouldn't talk about that.
Overpaid generic Gleevec, because look, I made, I made $5,000 on a single prescription for generic Gleevec and I said, how much, what does the pharmacist cost to dispense? It's around 10 bucks. Every state across the country shows the cost of Phillip prescriptions around 10 bucks. Now, look, let's just say it's a more expensive medication.
Maybe there's a little higher cost to dispense because you've got a higher inventory specialty product. Maybe you're calling Mrs. Jones to make sure she's okay. But an eight, $5,000 of a service. Okay. And so what we're speaking to is a broken incentive, because if, if the, if that pharmacy owner and look, I have full sympathy because that pharmacy owner has to deal with the $500 loss, the $600 loss, the hundred dollar loss, that $5,000 Gleevec is what's keeping the boat afloat.
I understand that, but we can't sit here as, uh, you know, as people saying, Hey, we want to change the system for the better and say, it's okay to have that poor. To over to over dispense a $5,000 product while dis basically giving all your other patients short shrift, because there are a bunch of losers.
What we should be saying is. Make the payment system agnostic from a drug category perspective. And if we want to inset pharmacists to do more, we do that through a separate clinical payment, whether it's through MTM or an actual, you know, billing code, like any other medical provider, but we should not agree with a system that arbitrarily can underpay 500 and then arbitrarily overpay 500.
Scott Knoer: Like Antonio said, there's some stuff when he started looking under the hood that isn't right either. And we have to acknowledge that and we have to be open to fixing the whole system. Um, but you know, I said about 5,000 times a day. Uh, our future Mike, uh, is about payment reform and we've got to change the insect.
Mike Koelzer: It seems with payment reform, it's all like chicken and a bunch of different eggs, you know, it's like, all right, Antonio, I'm not necessarily for the $5,000 upcharge, but it's like, I'll be damned if I'm, you know, if I'm a pharmacy talking who was maybe in that position, I'll be damned if I give that up though, before some of these improve, you know, and then they're not going to cut this price and only get it on the MTM, unless this happens.
It's so many chicken and eggs or.
Antonio Ciaccia: Totally, uh, Mike, what I listened to your more recent podcast with Envoy, uh, I thought, uh, did an excellent job kind of underscoring the need for realigning the incentive model and is something that's that Scott talks about, you know, all the time is, is it look. It's certainly a question of how much you paid.
Okay. But to me it's more about how you're paid and this is of the conversation I have with plan sponsors as well. You know, look, do you want your pharmacy to have those types of perverse incentives? Because if Mrs. Jones comes into Mike Kelsey's pharmacy with her generic. You better believe Kelsey's going to spend a lot of time with Mrs.
She might even get a free gallon of milk on the way out the door. Um, but you know, we want you to spend that extra time with a patient because you're actually bringing them to a, to an achievable and desired goal from a payment standpoint. It shouldn't just be based upon a roulette wheel of which patient walked through the door and got which prescriptions.
So, um, if we can realign that model to your point, it shouldn't just be. Cut off the $5,000 script and leave everything else the way it is. It's creating a system that creates a system that has a sustainable model for the dispensing function of the pharmacist, and then building added incentives on top of that.
But you've got to create the concrete first. So this, so this is something we talked about with state Medicaid programs. Do you want your pharmacy? To have this twisted incentive to, to, to take care of one patient over another. Do you want them to have [00:35:00] the lack of predictability? Because they're in these effective rate contracts where they're getting all this money taken back and they might get some, you know, add it to their, of their bank account.
Do you want to create a system that is a basic and simple cost plus model where the pharmacist has a reliable margin over the acquisition costs of their product? So they could serve each patient in an equitable manner and plan their business accordingly. And then once you have that system as trustworthy as it can be implemented within your practice or any other pharmacy practice, now we can talk about those other trinkets that we want to add onto there, whether it's immunizations, COVID testing, long acting, injectable products, MTM.
Ongoing chronic disease management. All of those things are possible, but no pharmacy owner can reasonably implement it with the chaos that is the bread and butter backbone of their practice. And that is the arbitrary PBM price setting for the dispensing of medication. In
Mike Koelzer: my simplistic mind, I'm just thinking, oh, okay, well, Antonio, that just hasn't happened yet.
Maybe because of the slowness of the government and so on. But in the other part of my mind, I got to imagine there's someone fighting against us, the AMA and the PBM, whatever the hell their initials are or something else who's fighting against clearing this up because we know down to the wholesaler. They love smoke and mirrors.
And I got to believe it's worse on the way up with the associations that maybe aren't on our side
Antonio Ciaccia: with mystery comes margin. Yes. Those that profit off mystery are going to oppose it. So obviously when we talk about moving to cost plus models in state Medicaid programs or in the commercial sector, The PBMs are huge opponents of that because their ability to manufacture price is what allows them to make unnecessary and undue gains off that, off that price.
So a major opposition from PBM associations and the PBMs. Insurance companies and the insurance companies, associations, um, wholesalers less. So, I mean, you would, you would, I know a lot of pharmacy owners, you know, think, you know, kind of looked down their nose at the wholesalers and granted there are problems.
There is no question, but I have not seen any, even, even close to the degree of opposition to pricing reforms in the drug channel, uh, from wholesalers or anybody else compared to the insurers and PBMs.
Scott Knoer: No, I absolutely do. And you know, and I'm working, uh, Antonio and I are working with, uh, some coalitions to try to get some money, to put toward legislation.
And I found the, uh, you know, you, you mentioned APCI so I think some of the smaller wholesalers. Very, uh, out to help pharmacists, you know, get reimbursed for the right things. Uh, and you know, we've, we've had, uh, all the majors. She helps wholesalers write pretty big checks to our coalition to try and get some provider status legislation passed.
No, Antonio, you mentioned insurance and sort of good and bad. You have had success in Ohio. And that's one of the reasons I brought you on. Uh, as my senior advisor insurance company, while they may have departments that don't get rewarded, you know, you've got the pharmacy benefit, but then you've got the medical benefit and, and demonstrating the
Antonio Ciaccia: value insurance companies and PBMs are going to fight tooth and nail to protect, protect their ability to artificially create prices on the distribution side.
So think about everything having to do with dispensing because that's where their money is. But. Look to the other end of that business model. So insurance companies, if you sit, if you were to sit down and say, what's the boardroom of a large insurance company look like they've got their PBM folks, they've got their, you know, plan sponsor folks.
They've got their medical benefit folks and their medical benefit could go for Medicaid, Medicare, commercial. Okay. They're CEOs for each one of those sectors, all sitting around that boardroom saying here's how, here's what, here's how I did last quarter. Here's how I did. We'll have Medicaid folks make money off of procuring Medicaid business in the states, in managing an overall benefit for those Medicaid beneficiaries.
Let's look at them for the sake of this conversation. Their job is to attract Medicaid members. Deliver a high standard of care, at least commensurate with what the state expects from a quality perspective. And then they also need to do so in an efficient way. Now meeting Medicaid members where their needs are, is very different.
Because they are a transient population. Often they lack adequate resources to achieve the goals that they need. And so oftentimes getting a Medicaid beneficiary to the goals that they have from a health plan perspective requires constant interaction and check-ins and care that is offered close to home.
Well, what the hell did I just explain? Except for far. Okay. Exactly. So [00:40:00] when I sat down with executives from United healthcare, a couple of years ago, you can imagine there was not a very friendly conversation at first, because of all the work that we've been doing on PBS. We said, let's take that conversation about the drug and put it off to the side.
Recognize me. We will not find commonality. Most likely there, let's talk about your problems. Let's talk about how you want to increase your enrollment. Let's talk about the members who aren't meeting their goals. Well, let me tell you about pharmacy, because while you have isolated the pharmacist under this pharmacy benefit and only looked at them primarily as a distributive mechanism for medication.
I'm here to tell you that you have a mental health patient, a diabetic patient, a hypertension patient, a cancer patient fill in the blank. That's walking through the doors of a healthcare facility. A pharmacy is a healthcare facility. They're walking through those doors at least once a month. You have the second, most educated healthcare professionals standing behind the counter.
They are overworked, overburdened, and they don't have time to engage that patient. So what we do is we have a technique. Take the 1520 medications and slide them across the counter and say, see you next month. What if we press pause on that, on that interaction and take that second, most educated healthcare professional out from behind the computer to talk to that patient, to see how they're doing wellness, check, check their levels, you name it, whatever it is, prompt them for a vaccination.
We don't have that in the model today. Because it used to be built into a lucrative dispensing model, which no longer exists because of everything that we put off to the side. So the question is you've got a member walking into that facility every month. Would you like to do something different and everything opened up at that point.
And so recognize it while pharmacists might look at those logos. And say, those are the bad guys, recognize underneath those logos is a tree and there's a lot of different branches that come off of that tree. The PBM is the largest branch and it can move the logo as a whole to recognize the CEO of the Medicaid plan has totally different incentives than what the guys over at the PBS.
Uh, are doing, and they have their own charts to the state because as we saw in Ohio, sometimes the PBM stuff can compromise the entire plan's existence in that state. And so the Medicaid CEO says, look, I understand they got to make Medicaid over. They got to make money over there, but what about us? And so it's that to say, look, the insurance companies are done taking advantage of the drug, but what I am saying is.
There are opportunities to meet these insurers where their incentives meet ours and pharmacists want to get paid more money to do better things for patients. So they could actually have the time to spend with those patients. Well, who can do that? Insurance companies who need healthcare providers closer to the patient's home, who can help them meet their, uh, healthcare and treatment goals.
Scott Knoer: I'm really glad Antonio brought that up. Cause this, this really summarizes, it summarizes the strategy that we're actually implementing. You know, it's three parts, it's all about payment reform. And, and part of that is, is the PBMs and the DIR fees. And what Antonio just described is like, I call it compartmentalizing because we're fighting PBMs for all those things for spread pricing, for DIR fees.
However, okay. We will work with the insurance covers. Owns the PBM to pay for the right things. And I have no problem, uh, you know, working with United healthcare or anybody that's going to pay pharmacists for the right things. We'll fight them in compartmentalizing. Mike, I think the analogy I use with that is me.
Nobody likes all of Scott right. But you might like minister, you might like that, but nobody likes all of me, you know, it's not like I had to like everything about you to work with you. I just got to go work for it. You know, but, but it is, it's, it's three parts and this is really important. Okay. You hear a lot about provider status, that's federal, right?
You understand that that's Medicare that's being recognized as a provider, but then it's, it's state by state. Okay. That's Ohio. That's why Antonio was here on this call with me because we worked together for that. And the third. You can't do without private insurance, right? So you have to have the value and the benefit, and I'm not aware of any other organization that gets that to the degree that we are, and that are executing.
I mean, we're helping our states, you know, we're fighting the PBMs, we're working for federal legislation and we are working with insurers, uh, directly in and attempting. States that are then they're paying in some states to move that across state lines. So it's, it's, you know, it's, it's not rocket science, right?
It's just, it's understanding the real issues and you can get off on just, you know, PBMs suck, which they do and all that. But, but, you know, we have to really look deeper and say, what can we control? Continue to fight there, but, but try to move the needle on the payment [00:45:00] reform. And that's the incentives
Mike Koelzer: when I'm talking to Doug from.
I think it was he that had mentioned that, look, there's going to be a big company. That's paying most of the pharmacy. I mean, it's that way across everything. There's only so many people like Amazon, there's Amazon and Walmart, and a couple other, I mean, there's always going to be a big company that conglomerates, so you're not going to like, get rid of that it's reform.
And what I love hearing from you guys is as pharmacists. Well, especially me. I like to bitch, I can bitch up a storm. That's cool. And I try to do something proactive with the beauty of the internet. You know, that's kind of why I did the podcast, you know, to get my voice heard and so on. But you just feel like you're little islands, but perhaps in my own little way, I've connected.
With you guys and in your listening and to all of us, it's just symbolic of that, but you're listening and you're taking it to some place that I really can't go. I mean, I can go maybe podcast wiser, but I'm not going to sit in the meeting with these guys or go to lunch with them in DC and things like that.
So it's a beautiful network. That's the importance of these organizations.
Scott Knoer: Well, Mike, you know, going back to your earlier Hamilton reference, right? I mean, that way you can kind of be in the room where it happens, influence and talk to folks, you know, which is very, very important.
Mike Koelzer: I don't know the history of the pharmacy organizations.
Did it take a lot of work for you guys to come together? Did you ever consider yourself like competitors among the other associations? Do you feel? You're working better than you have in the past, or has it always been a pretty good relationship and if it has changed, how did that change?
Scott Knoer: Yeah. You know, I've only been in this role for a year and a half or so.
Um, you know, philosophically with me. I will work with, uh, you know, all those organizations, APA was the original pharmacy organization. So everybody, at some point it sort of, you know, split off from, from a PHA. What we're doing now is having people come back and we work really well. I mean, Doug's a great guy.
You know, a lot of his members are my members as well. So Doug was out front on PBM reform. APH. I never really was into PBM reform until I showed up with Antonio and they were like, yeah, we get this. I had six and a half million dollars stolen from Cleveland clinic and DIR fees. Right. So, so. Uh, quite frankly, we just, Doug had a good strategy.
He said, Hey Scott, when I joined, I'm like, well, these are good things. So, you know, he was leaving the Rutledge versus PCMH. We filed an Amicus brief. He called it, this one's a little bit more expensive, but you know, we're suing health and human services. A lot of people know that it's NCPA versus Besera, but he asked were, was fun.
And 50% of that, I mean, we're spending hundreds of thousands of dollars to fund that. Working together. We jointly introduced a, a DIR. And then, uh, you know, we filed an Amicus brief for the North North Dakota farm association. Uh, so those are all things that we're doing together. Uh, but I, you know, that's, that's, uh, I'm working with Doug because that's his members, his board members are passionate about that.
I'm working with other organizations, you know, with ASAP the, our two organizations, um, got the bill introduced for the underserved areas. Now, lots of other folks are involved in signing on to that. But, you know, we work with, you know, every pharmacy organization, uh, out there on, on almost every foreigner's organization.
So I think, uh, the relationships are good. I don't know if there was ever animus. I don't know. Uh, there might be people, I don't see Doug as a competitor. I see him as a synergist. I want people to be, uh, NCPA members and APA members because you know, both of our organisms. Different angles and how we're doing things.
We work together on some things, some things Doug's board doesn't care about that we're doing. It's not that they're not the right things. It's just, they're not important to his board. Some things for ASAP are not important to other organizations. You know, if it's a pharmacy issue, it's important to EPHA.
So I work with every other pharmacy organization.
Mike Koelzer: Do you see most pharmacy organizations, even though they may not support something at all officially. Do you see any of the associations that don't agree inherently with anything? It seems like everybody's kind of on the same page. Is there anything that maybe a group doesn't agree with another group on in theory,
Scott Knoer: mostly, mostly same page, you know, they're there, uh, there's one group that.
You know, related to provider status, uh, I'm not going to name names. You're a smart guy. You might be able to figure it out, but am I going to throw stones? But, uh, there's one organization that apparently believes you have to have a PGY seven in order to talk to a patient. And they, they don't, they don't support provider says I [00:50:00] obviously exaggerated
Mike Koelzer: for effect there's organizations that think you need more education before you can use.
Well,
Scott Knoer: and I like to exaggerate for effect. So I have, uh, two residency's combined, so PGY one. That's okay. You get your pharm D postgraduate year one is a residency PGY one, and then usually some people can do a specialty. So if you want to do a general PGY one, and then you want to do oncology, that's a PGY two.
That's the most. Now I, you know, some of our clinical brethren, uh, sometimes think that they're the only ones that really understand patient care and those, those community pharmacists, they can do that, but they don't, you know, so there was one organization that did not, and does not support pharmacy provider status because they believe, uh, you have to be one of them in order to talk to a patient, I exaggerate for effect.
But so when you say. Most people, most organizations agree on everything. Yeah. I think most now care more about some stuff. So they put their resources toward it. This is one area where there's, like I said, one, one pharmacy professional society that I vigorously disagree with. I think every pharmacist out there, I mean, you know, we've all been Pharm D since what, 2 99.
And before that anyone that has graduated before has what? 30, some years of experience I could do the math. So I, I, our community pharmacists can provide clinical care. And so, when folks say you have to have this residency, you know, now if you're, you know, my previous place, Cleveland clinic, number one, heart hospital, the world.
Yeah. You probably need some specialized training, uh, to, to, to work in the cardiac ICU. But yeah, that's just me, uh, getting worked up over folks that think that our pharmacists on the front lines, uh, can only dispense drugs. That just grates mine, but you know, so it's sorry. I got a little worked
Mike Koelzer: up. All right guys.
So devil's advocate here. You're now the high-end mighty in Washington, DC and you've lost touch with us little people. And so, yes, maybe it's good that pharmacists should join a PHA, but the leaders now. Are losing touch. It's all theory. And so now we got to start over with some grassroots organization or something like that.
And Tony okay.
Antonio Ciaccia: No, definitely not. I, this is something I actually talked about at the state level, because we had some pharmacists that were, that thought, okay, Ohio pharmacists association, they don't represent me or they don't do a good enough job, whatever it is. They think that, you know, we've got the magic solution locked up in a storage closet somewhere and we're just unwilling to use it.
Uh, and they think, well, look, you know, I'll I'll get it. I'll get it done. I'll figure it out. I know, I know what's going on. I'll do it better than the folks in LA. And as to which I would say, look, if you think you're going to change the world for pharmacy. Okay. And this isn't to say you can't do it.
I was just going to say your chances are very low. All right. If you can't actually be involved within the Ohio pharmacists association, which is very easy to get involved in volunteering, join a committee, then maybe even join a board. If you can't even convince your own peers in that intimate setting within your own profession, that you're.
Good luck doing it outside of it. You're not going to, you're not going to.
Scott Knoer: Absolutely Mike, I got some thoughts on that too, you know, uh, some organisms and that happens in, in professional organizations, sometimes, uh, organizations run on inertia and all the organization cares about is for the organization to be successful.
That's not the way I think, you know, if we're not advocating for patients, you know, that's not good, but I also have a very strong board of directors that hired me. And I talked about diversity. You know, I have a Kroger executive, I have a couple of independent pharmacies, colleges of pharmacy.
They know the real issues. Right. We just had a board finance meeting. I learned so much, it keeps me sharp. Plus, you know, my girlfriend, she's, she's a pharmacy leader. She's practicing. Uh, I talked to, you know, folks, I did my Midwestern tour. I visited, I don't know, countless, uh, you know, pharmacies, um, you know, so it's yeah.
And do you want to? Filling scripts. You don't want me as your oncology specialist at NIH. Uh, but, but I, I get it, you know, and I feel the pain. So I understand what our folks are going through. I mean, we've got these crazies, my God, uh, telling the pharmacists, granted that's mental health, but you know that they're war criminals for dispensing or for immunizing.
And that one guy in Maryland, I mean, his brother-in-law. Clearly insane, but, but shot in the front lines, you know, it's just crazy stuff. So, uh, I never want to be so far from where I don't get it. And the other thing with me, Mike, you know, I got a five-year contract here. Uh, you know, you, you know, assuming I'm doing well and we like each other do another five, another five-year contract, but.
You know, [00:55:00] some folks get into a position where they're playing defense cave. All they want to do is not get fired. That's not me. If I were to play defense, just shoot me in the hand. I want to drive as hard and fast as I can all the time. So as long as I'm here at EPHA, we're going to be looking out for our patients and for our pharmacists, our profession in society.
There's no slowing down and no worrying about, Ooh, I don't want to do that. I might upset someone to ruffle some feathers because if I can't be effective in my role, find someone.
Mike Koelzer: I'm hoping to get fired from my pharmacy. I got to hire like a board that will oust me. I need, uh, in search Insta, get rid of me.
Scott Knoer: Yeah, exactly.
Mike Koelzer: Exactly. I follow this psychologist online and his big thing is. Clean your room. That's where you start. That's where the change
Antonio Ciaccia: happens. Everybody wants to change the world, but nobody wants to help mom with the dishes. Yeah,
Scott Knoer: exactly. Mike you're in Michigan, right? Yeah. So, you know, I hope to meet you in person at the Michigan farm association, uh, if I think February, I know it's winter.
I'm going to be the keynote speaker. Yes. If you get there, how can I turn it down? Detroit in February for God's sake and Carson, where else would I rather be?
Mike Koelzer: My dad always had insurance friends. They're having their annual meeting in Hawaii. It's like, why don't they go to Detroit in February? I think you were listening to my dad's conversation.
Well, it's funny.
Scott Knoer: I'm a car guy, right? So when I was in Cleveland, I'd always go to the Detroit auto show. And finally, of course they have it because COVID there. But finally now they changed it to June because January in Detroit was, you know, it's like, Hey, I love cars a lot now. So I went, thank
Mike Koelzer: God.
Is that something that's good for you to do? How often you get invited to those.
Scott Knoer: Oh, I love him. Uh, there's nothing I'd rather do. I've probably spoken at 20 states, you know, most of them were virtual, but I'm starting to do them live again. And again, that's the way to connect with members. The Florida pharmacy associates.
Was probably the first in-person one and, and you know what, I'm new. Everyone's like, oh, the new guys just like you right with the podcast. Now everyone's probably tired of me, but, uh, you know, but at least, uh, first they wanted me to talk. So I'm looking forward to the Michigan pharmacy association. You're doing
Mike Koelzer: great things.
Keep it
Antonio Ciaccia: up. Thank you, Mike. I'll keep listening to your stuff.
Scott Knoer: Thank you, my friend. Thank you.

Antonio Ciaccia
Consultant
Born and raised in the world of pharmacy, Antonio Ciaccia has been crawling around pharmacies his entire life. After three years as a pharmacy technician and two years of pre-pharmacy curriculum, Antonio diverted course, graduating from The Ohio State University in 2007 with dual degrees in communications and political science before moving into the world of association management, eventually heading up government affairs for the Ohio Pharmacists Association, where his data analytics work helped lead state officials to audit and uncover $244 million in hidden prescription drug overcharges in the state Medicaid managed care program.
After years of studying the pharmacy marketplace, Antonio became increasingly perplexed and concerned as he saw drug costs spiking while payouts to pharmacies were declining and more drugs were being excluded from plan coverage. Knowing something was being lost somewhere in the middle of an ever-growing transaction, Antonio has spent years working to crack the drug pricing code and pull the rug out from what he believes is one of the most dysfunctional marketplaces in the world.
Today, he serves as the President of 3 Axis Advisors, a consulting firm that works with Medicaid Fraud Control Units, provider groups, research firms, technology companies, law firms, investment analysts, employers, government agencies, benefit consultants, and private foundations to diagnose and eliminate inefficiencies and inappropriate incentives in the prescription drug supply chain. He is also the CEO and co-founder of 46brooklyn Research, a nonp… Read More








